Endometriosis, IBS and Diet: What you should know
Millions of women in Australia are affected by endometriosis and irritable bowel syndrome (IBS).
These are both ongoing, painful conditions with massive impact on quality of life.
Here we’ll outline the basics of each condition, look at whether the two conditions are connected and provide some tips on how to manage them.
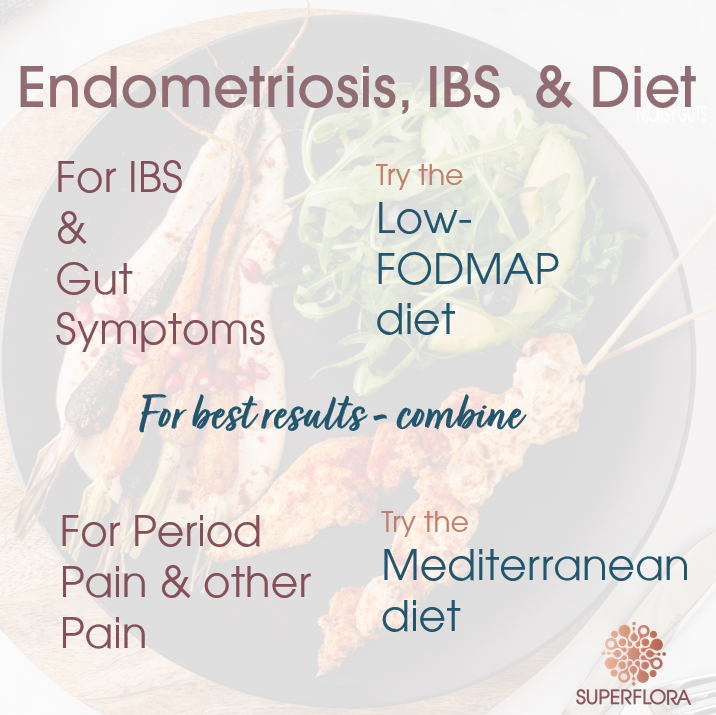
We look at a diet that can improve the IBS-type symptoms associated with endometriosis.
And we also explore other dietary changes that may help with the pain.
Sometimes it’s hard to be a woman
Both endometriosis and IBS are painful, ongoing, and debilitating conditions that can be difficult to talk about.
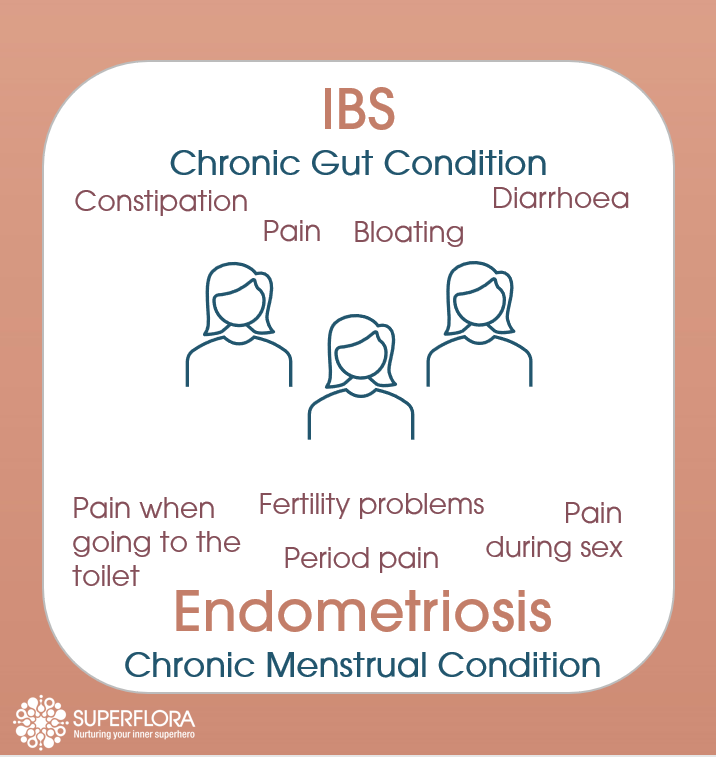
Endometriosis affects 10% of women. It occurs when tissue similar to that found lining the uterus (the endometrium) is also found outside of the uterus.
In the uterus, this is the tissue that grows each month to build a nourishing home for any new embryo. If no embryo embeds, hormone changes cause the lining to break down during the women’s period. In women with endometriosis, this cycle also occurs for the endometrial tissue found outside the uterus.
Surrounding tissues can become irritated and scar tissue can form. Endometriosis can lead to severe period pain, and pain during intercourse as well as pain when going to the toilet. It can also affect fertility.
IBS is also very common. It affects around 11% of the population, but is more common in women than men. Seventy per cent of people with IBS are women. It is often described as a disorder of the gut-brain axis: meaning that communication between the brain and the gut is out of kilter resulting in greater pain sensitivity in the gut, and changes in the rate of movement through the gut. Typical symptoms are pain, bloating and diarrhoea and/or constipation.
Do you have endometriosis or IBS or both?
Both endometriosis and IBS are difficult to diagnose. Laparoscopy (keyhole surgery) is needed to confirm endometriosis without doubt and there is no pathology test for IBS. IBS can be positively diagnosed using the Rome IV criteria, which is a series of questions about symptoms, but like endometriosis it is often diagnosed through an invasive procedure (in this case it’s a colonoscopy) to rule out other gut problems.
The two conditions also share some symptoms including abdominal pain, and often one can be confused for the other. There has long been a suggestion in the medical literature that the two may commonly co-occur, but it was difficult to tease the two apart.
To fully understand the pattern, the authors of a recent review carefully gathered and analysed many studies from around the world. They found that IBS is indeed more common in women with endometriosis. The risk of IBS is 3 times higher in women with endometriosis, and 50% of women with endometriosis meet the criteria for IBS.
The higher rate of IBS is not simply in women who have endometrial tissue associated with their intestines, but also women where this is not the case.
Given both conditions are difficult to diagnose, it is a good idea if you have had a diagnosis of IBS to get your doctor to check you carefully for signs of endometriosis, especially if your symptoms are worse around the time of your period or if you have a family history of the condition. Endometriosis can take many years to diagnose, but early diagnosis leads to better outcomes.
What causes the link between IBS and endometriosis?
More work is needed to answer this question, but it appears that both may have a common cause associated with inflammation and immune cells called mast cells and the chemicals they release. These have a range of effects including increased sensitivity of the internal organs and the pain experienced by women with IBS and endometriosis.
Challenging treatments
There is no cure for endometriosis. Standard treatments include hormone treatment and laparoscopic surgery to remove endometrial tissue. However, hormones are not useful for women trying for a baby or women who suffer side-effects. Similarly, surgery has it’s limitations - endometriosis can reoccur. Many women look for additional methods to reduce symptoms, including dietary changes.
Can the low-FODMAP diet help?
We’ve written a lot about the low-FODMAP diet. and how it can help many people with a range of gut issues. It was first developed to reduce IBS symptoms and there is growing evidence that the low-FODMAP diet can help around 70% of IBS sufferers.
The low-FODMAP diet involves removing a range of highly fermentable, short chain carbohydrates from your diet. This video explains more about it.
A study carried out in Christchurch New Zealand demonstrated that the low-FODMAP diet can help women with both endometriosis and IBS to improve their IBS symptoms. It appears that this group do even better on the diet than IBS patients without endometriosis. This was just one small study, but it is extremely promising.
What other dietary changes can you try?
A Swiss team published a big review last year looking at the evidence for a range of dietary changes that may help reduce endometriosis symptoms. They covered the New Zealand study on the low-FODMAP diet mentioned above, but they also found some possible benefits for supplementation with anti-oxidants like vitamins A, C and E and fish oils, although they concluded more rigorous studies were needed.
They were more confident at recommending The Mediterranean diet, in part because it is generally very good for you. They described a small Austrian study with 68 women who had persistent endometriosis symptoms after laparoscopy. They were asked to follow the Mediterranean diet for 5 months. The diet led to reduced general pain, period pain, pain during intercourse and pain when going to the toilet.
What is the Mediterranean diet?
The diet has the following elements.
Enjoy: ·
✅ Lots of fresh fruit and vegetables
✅ Pulses and legumes
✅ Cold pressed oils like extra virgin olive oil
✅ Wholegrains to provide fibre
✅ Oily fish
✅ Soy-based foods
✅ Nuts and seeds
✅ White meat
✅ Foods rich in magnesium
Avoid:
❌ Sugary drinks
❌ Red meat
❌ Foods high in sugar
❌ Foods high in animal fats
How does it work?
This bit isn’t really clear, but the diet is rich in vitamins and probably offers similar benefits to the anti-oxidant supplements mentioned above. The Mediterranean diet is also known to reduce inflammation, likely through the oily fish and extra virgin olive oil. For example, olive oil contains a chemical called oleocanthal, which is very similar to the chemical in ibuprofen and acts in the same way.
What are the other benefits?
A great thing about this diet is that it tastes so good, it is easy to stick to. You can flavour your food with lots of fresh herbs and spices.
Even if it does not improve your endometriosis, it is worth exploring for it’s many other health benefits including:
Boosting your microbiome
Reducing the risk of heart disease and strokes
Helping you live longer
Reducing the risk of Alzheimer’s disease
Reducing the risk of Parkinson’s disease
Protecting against type 2 diabetes
A winning combination?
Make sure to talk to your doctor about the best treatment plan for you, but if you have endometriosis and IBS, it may be worthwhile giving the low-FODMAP diet a go.
It is also worth experimenting with the Mediterranean diet as a way to reduce the various types of pain caused by endometriosis.
These diets won’t cure endometriosis or IBS, but they may well impove your symptoms.
Resources
We are big fans of both diets and the recipes on our site combine elements of both.
A good place to start would be our Good Gut Challenge. It incorporates a 10 day meal plan including our low-FODMAP Superflora Gut Health shakes.
Written by: Dr Mary Webberley, Chief Scientific Officer at Noisy Guts. Mary has a background in biology, with two degrees from the University of Cambridge and post-doctoral research experience. She spent several years undertaking research into the diagnosis of IBS and IBD. She was the winner of the 2018 CSIRO Breakout Female Scientist Award.